Part One: Functional flat feet, collapsed arches, ankle deformities
The feet serve as the foundation of the human body. Deformities and misalignment in the ankles can lead to a cascade effect, affecting the alignment of various body parts from bottom to top, resulting in issues such as functional leg length discrepancies, pelvic tilting, and consequent misalignment of the spine (functional scoliosis). This can cause issues of excessive tightness or relaxation in muscles, ligaments, and soft tissues, misalignment or compression leading to wear and tear in joints, improper deformation due to undue stress on cartilage, nerve compression, and so on...
If the body's skeletal structure is misaligned, it can create an imbalance in tension on both sides and front and back muscles, leading to compensatory movements and, over time, causing various pain issues such as limb soreness, body soreness, shoulder and neck discomfort, and degenerative joint arthritis due to wear and tear.
Functional flat feet, collapsed arches, and foot deformities can also weaken the employment of muscles in the sole, subsequently leading to the weakening of lower limb muscle strength (especially the adductors muscle group), pelvic floor muscle group, and core muscle group. Compensatory forces from other muscle groups or soft tissues can result in a tense state, causing the loss of original elasticity and extensibility (such as the iliotibial band).
In dynamic movements, functional flat feet, collapsed arches, and foot deformities can cause the human body to sway and tilt more, generating unnecessary tilting pressure and wear on joints and cartilage, or leading to misalignment. Therefore, the stability of the feet, whether in static or dynamic operations, is crucial for the human body!
In ancient times, the terrain was softer, consisting of sandy, grassy, or muddy ground. When stepping, the outer side would sink, forming a beautiful footprint. This allowed the inner arch of the foot to take shape without collapsing. On terrain suitable for human feet, which is slightly softer, the muscles on the sole would be fully trained. When the sole muscles contract, they connect to the muscles on the inner back side of the lower limbs, promoting the contraction of the core muscle group and enhancing core muscle strength.
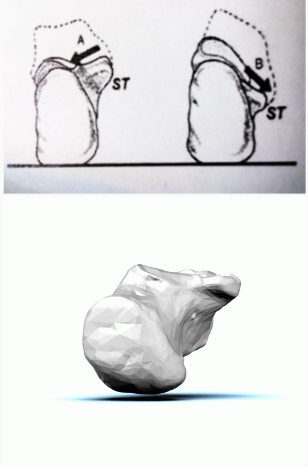
Nowadays, every inch of the land is hard. When people, especially toddlers whose arches have not yet formed and whose muscle strength is insufficient, start standing and walking on flat, hard surfaces, the outer side of the foot arch cannot sink into the ground. The muscles in the lower limbs are not yet strong, and the arch on the inner side of the foot is prone to collapse (the sustentaculum tali of calcaneus tends to inward collapse and deform, the navicular bone along with the cuneiform bones collapses inward, misalignment of the subtalar joint, causing a series of misalignments in bone joints and deformations in the bones and joints.
Additionally, modern shoes with increasingly protective and enveloping designs limit the use of toes and sole muscles, making it more challenging for the arch to take shape. In the past, corrective insoles primarily provided passive support with a certain level of hardness in material and various shortcomings. For more details, please refer to the video link and the winning comparison table in the GIMIALIGN AI 3D Smart Socks (attached video link).
Part two: Functional flat feet lead to biomechanical misalignment in the lower limbs
The proper arch of the foot presents a straight line formed by the tibia, subtalar joint, and the foot (second phalanx bone). Assuming the arch of the right foot collapses inward and the scaphoid bone drops, resulting in functional flat feet, the muscles and fascia on the sole of the foot will be stretched, increasing pressure. The originally straight line formed by the tibia, subtalar joint, and foot will become curved, leading to an inward rotation of the thighs and shins, forming an X-shaped leg alignment. Due to the greater internal rotation of the lower leg compared to the thigh, the anterior cruciate ligament is pulled forward, the medial collateral ligament is stretched, and the outer part of the meniscus cartilage is compressed and worn down.This also explains why many people experience more severe unilateral knee/hip joint degeneration.
In general, the knee joint is typically required to bend beyond 55 degrees before wear and tear affects the central meniscus. However, when X-shaped legs form, incorrect compression of the knee joint can lead to potential abrasion even before reaching 50 degrees. Moreover, during rapid movements, braking, or sudden stops, the ligaments attached to the meniscus cartilage may be subject to stretching and tearing.
Furthermore, with the development of X-shaped legs, the iliotibial band and vastus lateralis may shorten and contract, resulting in iliotibial band syndrome and lateral patellar lateral tracking. The patella may shift outward and upward, causing patellofemoral syndrome and lateral patellar tracking. Additionally, when the knees are rotated outward in X-shaped legs, the patella does not slide along its normal track, leading to abrasion and chondromalacia of patella.
As mentioned earlier, when the bones of the thighs and shins rotate inward, X-shaped legs are formed. If the angles at which the arches of both feet collapse are different, the inward rotation of the thigh and shin bones will also differ, causing asymmetry in the lengths of the lower limbs. This results in functional leg length discrepancy. Therefore, simply elevating the shorter side with corrective insoles without addressing the overall skeletal alignment and relaxing soft tissues is absurd. Once the entire skeletal structure is adjusted, and the feet support the symmetrical and correct arch angles, the natural resolution of the length and height equality of both sides can be achieved.
After the formation of X-shaped legs, the iliotibial band tightens. When this happens, it pulls down the gluteus medius and tensor fasciae latae muscles. Since the gluteus medius is crucial for the biomechanical strength and movement of the lower limbs, when it is pulled down, the time for it to contract back after being stretched is prolonged, leading to delayed activation. This results in increased body sway, a longer and slower transmission path of force, increased compensatory movements, and greater stability control burden. When every movement of an athlete is delayed by fractions of a second, the overall speed decreases. In clinical practice, after adjusting the overall skeletal and joint alignment and strengthening weakened muscle groups through induced training, the use of corrective insoles has been observed to enhance athletic abilities, increase speed, and eliminate compensatory muscle contractions and movements. Additionally, when the spine compensates for scoliosis, adjacent nerves may be interfered with due to narrowed spaces or tense soft tissues, causing slow nerve signal transmission and possibly nerve symptoms or pain due to compression.
Part Three: Functional Scoliosis
Continuing from the previous section, when both thighs rotate inward, the femoral heads of the human body will tend to move backward to the concave of the pelvic bone (acetabulum). This backward movement causes external rotation and anterior tilt of the pelvic, leading to the misalignment of the sacroiliac joint and contraction of the piriformis muscle. As the sacroiliac joint misalignment persists, and the iliolumbar ligaments become lax over time, coupled with pelvic tilt and uneven height, the spine begins to compensate by developing lateral bends, which is one of the reasons for functional scoliosis and uneven shoulders.
Scoliosis also results in different tension levels in the muscles on either side of the spine. Muscles on the concave side of the back are typically tighter, while those on the convex side are more relaxed. The tense area on the concave side corresponds to the relaxed area on the convex side in the front.
The spine is a crucial support structure for the skeletal framework of the human body. In a normal situation, the spine appears straight when viewed from the back. However, when the spine forms one to three curvature angles, accompanied by vertebral body rotation, it results in a C-shaped, S-shaped or C+S-shaped curvature when viewed from the back. The convex side of the spine exhibits protrusions or height differences in the lumbar, thoracic, and cervical areas, causing pelvic rotation and tilt. When the body bends forward, there is a high-low appearance on the back, known as scoliosis. Additional visible effects include uneven shoulders, tilting of the head and neck, and one-sided rounded shoulder with the scapula protruding.
Some cases of scoliosis are congenital (idiopathic scoliosis), and modern medicine still cannot pinpoint specific reasons for them. However, a significant number of people may develop acquired functional scoliosis due to issues with the feet, leading to pelvic and skeletal joint misalignments and imbalances in posture. This can result in muscle weakness, pathology, and degeneration.
Whether scoliosis is congenital or acquired as functional scoliosis, it not only affects the body's appearance but also tends to increase in angle with age (1. Adolescence is the stage of the most significant angle increase; 2. Entering old age with osteoporosis and bone-joint degeneration is the second-largest stage of angle increase). Scoliosis can cause back pain, herniated discs, spondylolisthesis, compression fractures, or muscle weakness in certain muscle groups. As the angle of scoliosis continues to increase with age, severe cases may lead to nerve compression around the spine or visceral compression due to deformity in the ribs/chest.
Scoliosis is a symptom with a progressively increasing curvature angle. Early intervention for scoliosis patients yields better corrective results. The adolescent growth stage is when scoliosis angles change the most. Regardless of whether scoliosis is congenital or acquired as functional scoliosis, early assessment and wearing corrective braces are the most effective interventions.